The social, health and economic burden of non-communicable diseases (NCDs) to the South African economy and social fabric has not gone unnoticed. South Africa has frequently updated its strategies to combat NCDs in order to slow and even reverse the impact of NCDs on its GDP over time. In this blog we outline more recent NCD action in South Africa, research to support the action, and recommendations that consider where implementation is challenged and concerted efforts are needed to advance a multi-level, multisectoral, and multi-actor integrated approach.
The importance of NCD action in South Africa
Addressing NCDs is a veritable challenge, everywhere. The growing burden of NCDs in South Africa led to political commitment from the government at the UN High Level Meeting on NCDs in 2011. South Africa enhanced its efforts by developing the National Strategic Plan for the prevention and control of NCD 2013-2017 followed by the National Strategic Plan for the prevention and control of NCDs 2020-2025. This strategy aims to assist South Africa in achieving Target 3.4 (By 2030, reduce by one third premature mortality from NCDs through prevention and treatment and promote mental health and well-being.) of the Sustainable Development Goals (SDGs). It will simultaneously address several other SDGs that are impacted by NCDs.
In order to support evidence-informed interventions and approaches to NCD prevention, research and implementation teams have partnered across the country to provide the government with context relevant evidence to guide decision-making. One such research consortium is the Collaboration for Evidence-based Healthcare and Public Health in Africa (CEBHA+)1.
Research to guide NCD action in South Africa
CEBHA+ (2017-2023) aimed to establish long-term capacity and infrastructure for evidence-based healthcare and public health in sub-Saharan Africa, to strengthen African research institutions, and to build competence in the understanding and rapid uptake of evidence in health system institutions. In South Africa, three institutions, Stellenbosch University, Cochrane South Africa, and the Chronic Diseases Initiative for Africa (CDIA) worked together to produce research evidence, and translate these into policy and practice implications for key NCD stakeholders.
Oftentimes research teams do great research but fail in terms of sharing that information appropriately with the intended users. The CEBHA+ team incorporated an Integrated Knowledge Translation (IKT) approach, which engages stakeholders throughout the research process – from priority setting to results integration – and ensures that the evidence is tailored to the various end users.
In South Africa, the CEBHA+ team focused on research related to screening of diabetes and hypertension, integrated models of care for diabetes and hypertension, and population level interventions to prevent diabetes and hypertension. These were all priorities identified in collaboration with the Western Cape and National Departments of Health at the start of the project and aligned well with the NCD strategic plan of the time. The results of these studies were shared through meetings, conferences, academic peer reviewed publications, issue briefs and policy dialogues. Understanding how IKT was employed to advance noncommunicable disease policy and practice in South Africa can be found in the link.
Issue Briefs for policy and practice: a tool for communicating action
Given that most research is not packaged for decision makers, doesn’t include suggested action items, and often ignores the real-world implications of these actions, the CEBHA+ team summarised the various studies into Issue Briefs that highlighted the problem, the suggested solutions and the implications of those actions.
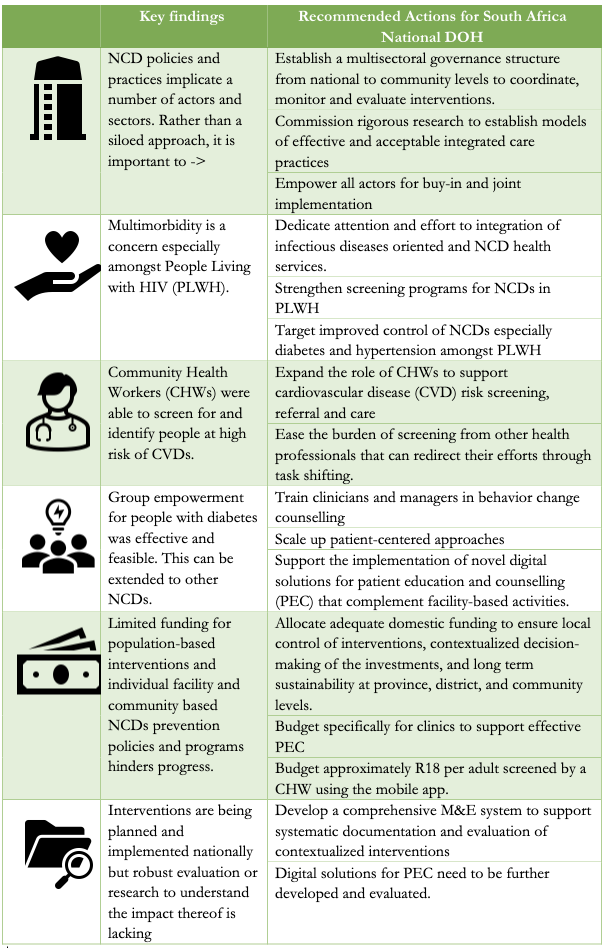
What was found and what needs to be done by the National and Provincial Departments of Health in South Africa?
The various research implicates different actors and stakeholders. For the Departments of Health it is imperative to understand the results and what actions are required on their part.
Implications for implementation
-
Much of this is only going to be possible using a multisectoral approach.
-
Engagement of stakeholders from all levels of policy making, prevention, and management form the onset of the planning stages to ensure appropriate and effective implementation.
-
Partner with researchers and funders to ensure that planned and ongoing programmes are evaluated adequately to inform future cost-effective policies. M&E requires involvement across sectors.
-
The health information system should document the reach of effective PEC and the medical record should record what PEC has been given and support continuity of care.
-
Increase the health workforce: E.g., Approx 450CHWs per million are needed to screen the entire adult SA population for CVD. (~20,000 CHWs of the 700,000 CHW positions proposed by the South Africa National Planning Commission.)
-
Buy-in from a variety of actors will require genuine and authentic engagement
-
Address challenges experienced at primary health care level such as staff shortages, drug stock-outs and malfunctioning equipment, to ensure sustainability of integrated care.
-
Primary care providers will need training to be experts in NCDs, lifestyle modification and communication skills that motivate and empower patients.
-
PEC will need to be supported by the necessary educational resources and supplies.
We recognize that there is other evidence that needs to be considered and that there may be updated data since the time of this research. While it is unlikely that the above recommendations and implications will be a surprise for the NDoH, we urge key decision-makers to be guided by the evidence to implement action and consider the implications of these. Else, we will once again be creating the next strategy with the same concerns and the same assertions but without enough progress from the years past.
The question is: will these results, and those of other research teams, compel action so that we move beyond intention and implement change? Let’s hope so!
For access to the full Issue Briefs written during the project period see links below:
For access to peer reviewed publications linked to each of these issue briefs see the CEBHA+ website.
Acknowledgements: The author would like to thank Anke Rohwer, Peter Delobelle and Taryn Young for their contributions to this blog. The research mentioned in these issues briefs was funded by the German Federal Ministry of Education and Research.
About the author: Dr. Nasreen Jessani is a senior researcher at the Centre for Evidence Based Health Care at Stellenbosch University in South Africa, and Associate faculty at Johns Hopkins School of public Health. Her focus is on the nexus between health policy and systems research; innovations in evidence-informed policy and practice; knowledge translation and brokering, and the relationship between academia and public policy. She currently serves on the advisory board for INASP, UK and AcademyHealth, USA.; the Canadian Association for Global Health, Canada; the Forum for Health Professions Education at the National Academies of Sciences, USA, and the WHO EVIPNet Global Steering Group. She is also on the Steering committee for World Evidence-Based Health Care day, and Associate Editor of Health Research Policy and Systems Journal. Nasreen was previously the Head of Strategy for the Africa Evidence Network and a Program Officer at Canada’s International Development Research Centre (IDRC). Nasreen holds a DrPH (Johns Hopkins University), MSPH (UNC-Chapel Hill), BSc (McGill University). You can contact her on LinkedIn and/or on Twitter.
Disclaimer: The views expressed in published blog posts, as well as any errors or omissions, are the sole responsibility of the author/s and do not represent the views of the publisher, its secretariat, advisory or reference groups, or its funders; nor does it imply endorsement by the afore-mentioned parties.
